Jordan and Chris became parents on December 19, 2022. I loved getting to know them over the course of my 7-week childbirth series and grew excited for the opportunity to attend their birth. Jordan was due near the holidays and she and Chris hired me knowing I had travel plans. They trusted they would be in excellent hands in the event of a backup doula, but as the due date drew closer and Jordan was not showing any signs of labor, she felt more and more comfortable with an induction.
Jordan wanted to wait beyond her due date but was comfortable with an induction at 41 weeks to insure her chosen people would be present: her doula, her mom, and other family members who had traveled from Africa and were scheduled to leave on the 20th. The date was put on the calendar for a Sunday night ripening on Dec. 18, and induction the next morning since she was only dilated 1 cm.
Jordan checked in for induction and her body had made some big changes since her previous appointment. Jordan was dilated 4 cm and 80% effaced, and she was already having contractions! Just like that, the plan changed from ripening overnight to a full-on induction. The plan was to begin Pitocin in about an hour or so.
In a surprising turn of events from my end, I was at another birth.. It had been a drawn-out ripening and induction that spanned the weekend and while we were hopeful for a baby in the early morning hours, we couldn’t know exactly when. In spite of best laid plans to schedule an induction to assemble her birth team, Jordan was likely going to have a backup doula anyway. I am so grateful for steady backup support and so were Jordan and Chris. They continued with the induction plan trusting it would all work out as it was meant to. I contacted my backup doula, Liz to get her in the loop with what was going on so she would be ready to possibly get called in. All of this came together around 8:30 pm on Sunday.
Three hours later, just before midnight, Chris texted to say that Jordan was dilated 4-5 cm with contractions coming 3-5 minutes apart. The Pitocin had taken hold but Jordan continued to breathe calmly through each contraction and was coping well, so they didn’t feel it was quite time for doula support.
Two and a half hours after that, around 2:00 am, Jordan’s water broke. She was still dilated 5 but the intensity of the contractions was ramping up. I was with my other client who was pushing, but it was looking like time to call in backup. Within 10 minutes, they reached out to Liz who was soon on her way to the hospital to support them.
Jordan’s labor took a very active turn with long and strong contractions that were hard to stay on top of. She decided to get an epidural in the hope she might get a break before it was time to push. She was exhausted. By 3:30 am, once comfortable from the epidural, an exam confirmed it was a good decision since she was still dilated 6 cm, 90% effaced, and baby was at -1. Jordan was eager for a nap and it was looking like she had time to get one.
Within the hour Jordan was dilated 7.5 cm and 100% effaced, and her baby was coming down well. I was still with my other client so it was still up in the air whether I would make it. But Liz was holding down the fort and providing excellent support. An hour later, upon feeling lots of pressure and with some bloody show, Jordan got checked and was dilated 9 cm! Her body had taken off. Some creative positioning with the bed had her upright to help her cervix melt away and bring her baby down.
Having welcomed a baby with my other client, I was able to come support Jordan and Chris in the last part of the birth. (It helped that both clients were birthing at the same hospital!) We were all very grateful for Liz’s 2+ hours of support in the meantime. I joined them just before 5:30 am.
Jordan’s nurse had been very diligent about coming in every 20 minutes to encourage position changes, and with Liz’s help she was already very close to pushing. Jordan was feeling some pain in her right hip and back, so I prepared a heating pack for some relief.
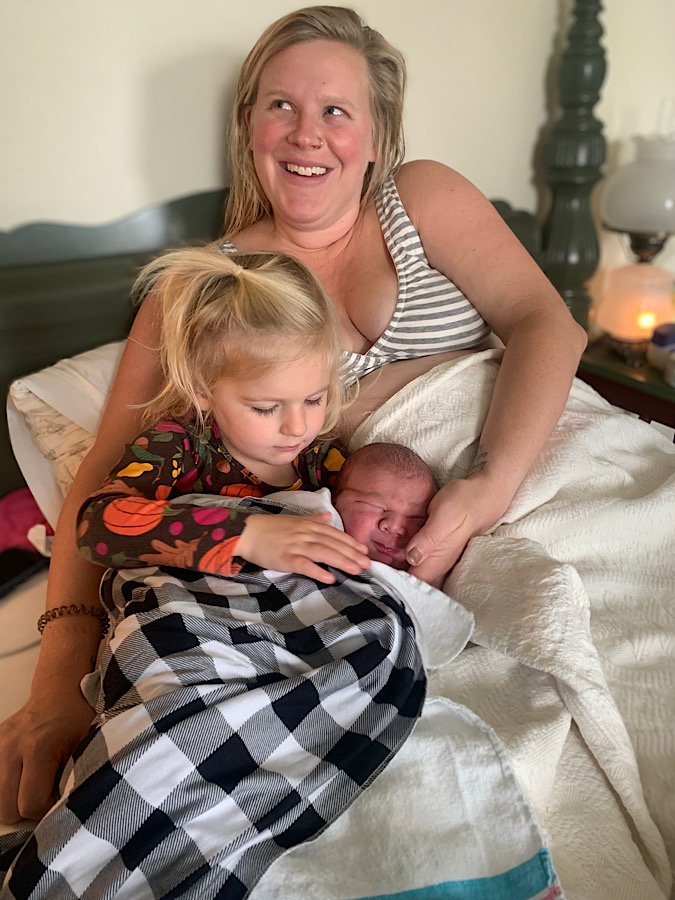
The midwife came in and did an exam and was excited to find that Jordan was completely dilated. At 6:15 am Jordan gave her first pushes to see how her baby moved. Her midwife was very pleased with her pushing, so she remained in the room and had Jordan continue. With her mom on one side, and Chris on the other, Jordan pushed with each contraction and moved her baby down so well. We saw her baby’s dark hair by 6:45 am and at 6:52 Jordan reached down and felt her baby’s head with her own hand. (I just love to see the reactions of moms when they do this. Their eyes are always wide as saucers!) Then at exactly 7:00 am Jordan pushed her big girl, Sahara Rose, out into the world! It was December 20, and ironically at right about the time the induction process was originally scheduled to begin.
There was so much love in that room! Jordan’s nurse had made a deal with Sahara that she WOULD be born ON her shift, and we all laughed to see that she did just that. Nurses are priceless, especially when they connect so well with their patients. Sahara was a gorgeous baby, and the added chunk only made her more so. She had a head full of dark hair and a sweet disposition from the start. Jordan and Chris were immediately enamored with their daughter and doted on her little parts and the wonder of how strong she was, lifting her head and grabbing fingers from the start. And as if her neck roll didn’t already give her away, her strength did, because she weighed a hefty 9 lb. 3 oz.! No on expected that, least of all Jordan. But it just goes to show that her body was made for it.
Jordan had eager family in the waiting room who came in to meet sweet Sahara Rose. She was the first grandchild on both sides, so she was obviously much anticipated. I gathered my things to leave after the initial hour. I knew after the euphoria wore off a bit, she would be hungry and tired. But the euphoria was contagious as I left the room. The blessing of two babies born so close to Christmas, ignited the anticipation I had for seeing my own family over the holidays. And I was grateful the babies had spaced themselves in such a way that I could attend at least some of Jordan’s birth.