Devin and Ben welcomed their third baby girl, Austin Elizabeth, on November 15. Davin’s births were all very different. Her first was a c-section, the second was a VBAC (and she arrived at the hospital ready to push!), and this was a second VBAC! However, it wasn’t without its challenges. This time around, Devin’s placenta had a velamentous cord insertion which can leave the vessels more vulnerable. There is not a lot that can be done except possibly induce a little early to protect baby from an incident, albeit a rare one.
But Devin’s baby was also measuring smaller, and her growth had dropped to an alarming threshold, which had her providers recommending induction. Her baby remained steady in growth and even had a little growth spurt, but between the VCI and her baby falling low on the growth chart, an induction was the decision agreed upon. It was scheduled for 39 weeks, so not terribly early.
Devin was dilated 2 cm at the start of the process. She was no stranger to unmedicated birth, but this would be her first time with pitocin, so it would still be a new experience. They got situated that morning and once she was admitted, the plan discussed, and everything began, it was later in the morning. There was not much of an update since nothing much was happening initially. It took awhile for Devin’s body to respond with contractions and when it did, she was dilated 3 cm, so she went into the shower.
In fact, Ben’s first update came at 2:47 pm saying “the contractions were more intense, and he was helping to squeeze hips for help on the contractions.” When I asked how far apart and how long they were, he responded that they weren’t long and two minutes apart. It soon became clear that it was time for me to head in.
Devin didn’t know if it was quite time, but she was breathing through the contractions. The pitocin was at 12 mu and by the last text, Ben confirmed the contractions were close to 60 seconds and 2 minutes apart. I was dressed and packed so left the house shortly. I arrived 20 minutes later at 3:37 pm. And Devin had emerged from the shower a short time before I arrived. She had dilated from 3 cm to 8 cm in a very short time!
When I walked in, it was evident that Devin had turned a corner quickly. Her midwife was present, and she was struggling to stay on top of her contractions. She had asked for an epidural, but the simple fact of the matter was that she didn’t have time. Plus, it was not what she initially wanted. Ben pressed on her hips during contractions, and I took my place beside them to offer encouragement to Devin.
We kept her focused on one contraction at a time and she breathed through her contractions courageously. Her cervix was changing rapidly. She was already dilated 8 cm and it was only a matter of time before her body would lurch her into a push. In the meantime, she was wavering and not sure how much more stamina she had. She agreed to have her midwife break her water in the hopes that the last bit of cervix would melt away as baby came down. But it didn’t go quite like that.
Devin had a rim of cervix that remained through several contractions. Her midwife offered to push the cervix aside during a contraction to help Devin with dilation to complete and she was game. This is not a pleasant thing to go through, but Devin faced it head on and like a champ. And she was fully dilated as a result. Devin labored upright in the bed, pulling on the rebozo tied to the squat bar, and she soon felt the familiar sensations of a baby coming.
Devin pushed on her hands and knees over the CUB. She pushed quietly and with great strength and it didn’t take long at all for us to see her baby’s head. Austin Elizabeth was born at 4:26 pm with a full set of eye lashes! The midwife passed her through Devin’s legs and up into her arms. Devin hugged her close and cried with joy to know her littlest girl was safely born.
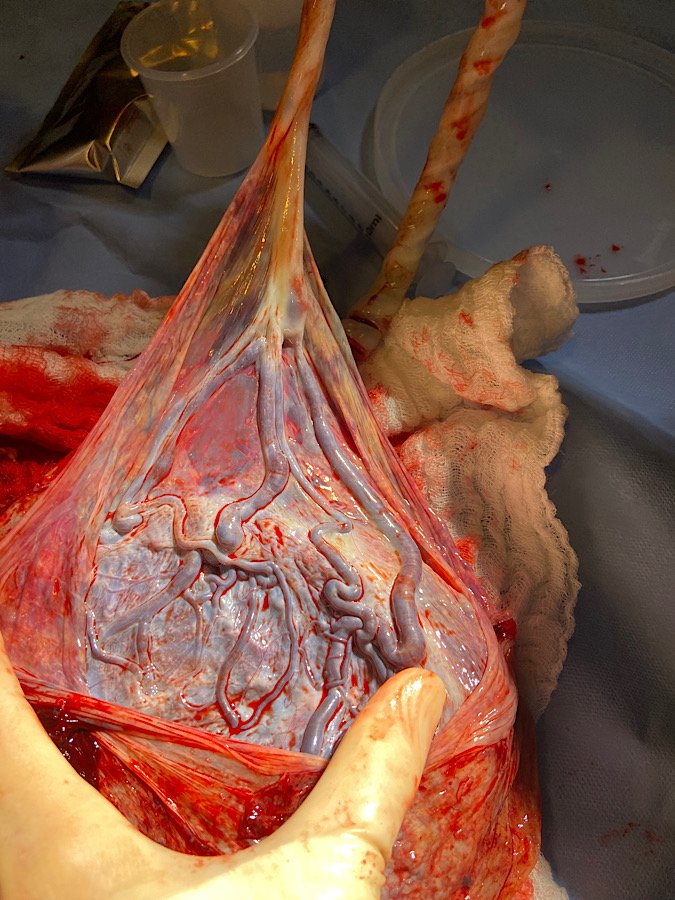
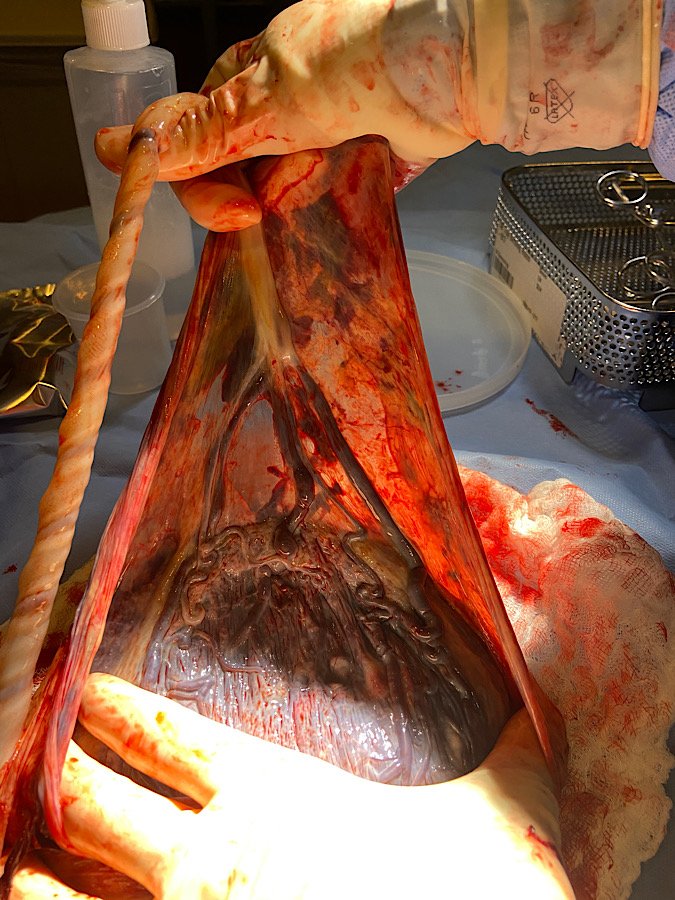
The placenta was a sight to see, and we took many pictures of the rare velamentous cord insertion. Austin snuggled with her mommy and soon got skin to skin with her daddy. She was small, weighing just 6 lb. 2 oz. but it wouldn’t be long before she got chunky on her mom’s milk.
Devin’s labor was such a joy. She welcomed her baby with glee and had a wonderfully flexible approach to the birth. And when induction became the plan, she rolled with that too. Pitocin is no joke, but Devin rode those rocky waves with such courage. I’m very proud of her as should she! And now she is a member of the 2VBAC club!